The Mysteries of Chronic Illness

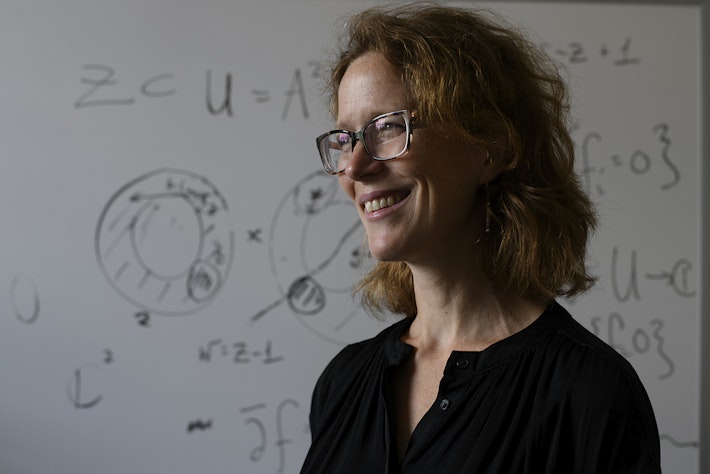
Meghan O'Rourke’s book on chronic illness will weave together her own experience with cultural criticism and medical journalism.
Baby bees stinging her whole body.
That was the first symptom Meghan O’Rourke RI ’15 experienced in 1997, when she was 21. As abruptly as the stinging began, it would end. Later she was attacked by hives. At one point, she was diagnosed with lupus, but it turned out she’d been misdiagnosed. These episodes plagued her for years and seemed to come out of nowhere.
After a bookish childhood in Brooklyn—where her parents, free spirits of the ’60s and ’70s, taught at a private school, St. Ann’s—O’Rourke attended Yale, where she collected a raft of awards for her poetry, fiction, and nonfiction. After college she worked at the New Yorker, first as an assistant to the editor Bill Buford, and then as a fiction and nonfiction editor, one of the youngest ever hired.
She moved to the online magazine Slate, where she created the culture and books section, and also worked part-time at the Paris Review, where she served a five-year stretch as poetry editor. In 2005 she earned an MFA in poetry at Warren Wilson College, and in 2007 she began teaching poetry, first at the New School, then at Princeton, where she continues to teach undergraduates, and then at New York University, where she’s now an associate professor in the graduate writing program.
Through all this—sickness and health, school and work—O’Rourke wrote and wrote and wrote. By 2012 she had published more than 100 articles and three books—two of poetry, Halflife (Norton, 2007) and Once (Norton, 2011) and one of nonfiction, The Long Goodbye: A Memoir (Riverhead, 2011).
The memoir is O’Rourke’s chronicle of what happened to her family after her 53-year-old mother was diagnosed in 2006 with stage IV colorectal cancer. O’Rourke’s parents had moved to Connecticut by then to work in a new private school. With O’Rourke and her two younger brothers off on their own, their parents were starting a new life, but now it was coming undone. O’Rourke’s mother underwent chemotherapy and her cancer was briefly in remission, but it returned and moved fast. She died at home on Christmas Day in 2008.
O’Rourke’s medical symptoms began to intensify in the year after her mother’s death. She suffered overwhelming fatigue, aching lymph nodes, fever, headaches, and rashes that doctors couldn’t explain. Eventually a specialist in women’s health diagnosed her with autoimmune thyroiditis, or Hashimoto’s. But replacement thyroid hormones didn’t bring relief. O’Rourke began looking online for information about Hashimoto’s and other autoimmune diseases.
In an essay published in the New Yorker, she describes her disabling symptoms, her quest for a diagnosis, and the alarming rise of autoimmune disease among women. “Today, researchers believe that they have discovered some 80 to 100 autoimmune disorders,” she writes, “including disorders as various as lupus, multiple sclerosis, type 1 diabetes, and rheumatoid arthritis.” And three-quarters of autoimmune patients are women. It’s one of the most prevalent categories of disease, ahead of cancer. When O’Rourke finished the article, she felt she had just started exploring the subject.
She had intended to make her next book about young women and gymnastics, a subject she knows from experience, but now she changed course. She would braid her personal experience of chronic illness with an investigation of the ways the medical system is challenged in caring for people with these maladies. She signed a contract with Riverhead to deliver the manuscript in September 2016.
Fortunately, in the fall of 2013, O’Rourke received the diagnosis that eased her symptoms. A doctor tested her for Lyme disease and its co-infections and gave her several rounds of antibiotics and anti-malaria drugs, and she began to feel better. But her cure is not complete: she still suffers from three autoimmune disorders and her neurological damage seems to be worsening.
Student Researchers
At the Radcliffe Institute, where O’Rourke holds the Helen Putnam Fellowship, she has dived into research for her book, with help from four undergraduate research partners. “They’re incredibly smart and energetic,” she says. “One of them made a chart on simplified immunology for me, because I’m an English major. The book will be so much better for having their help.” The students each work four to six hours a week and meet with O’Rourke as a group—seminar style—to discuss their findings.
When she’s not meeting with students or conducting interviews with scientists and people with autoimmunity, O’Rourke is fully immersing herself in the Harvard experience: attending Helen Vendler’s poetry classes (“She’s wonderful—an intensely penetrating reader,” O’Rourke says of the Arthur Kingsley Porter University Professor) and as many lectures and talks as she can (such as a climate-change symposium at the Woods Hole Oceanographic Institute led by Amala Mahadevan RI ’15, who is a scientist there).
In an Atlantic essay published this past November—“Doctors Tell All—And It’s Bad,” on which she worked with the editor Ann Hulbert ’77—O’Rourke reviews a new crop of books by physicians in which they reveal their disillusionment with the healthcare system. The books include What Doctors Feel: How Emotions Affect the Practice of Medicine, by Danielle Ofri (Beacon Press, 2013). “After reading these books in the aggregate, you realize how psychologically taxing it is to be a doctor,” O’Rourke says.
“I’ve now learned that patients aren’t alone in feeling that doctors are failing them,” she writes in the essay. “Behind the scenes, many doctors feel the same way.” She reports, for example, on Ofri’s belief that empathy gets in the way of what doctors must do to survive, even though empathy can be essential to healing. Ofri found that patients with severe diabetes whose doctors rate high on a standard empathy scale have 40 percent fewer complications.
O’Rourke stresses the importance of empathy and acknowledgment of physical symptoms for people with chronic disease. “If people are having vague but distressing symptoms,” she says, “they don’t need other people to say ‘Are you depressed?’ Maybe they are and maybe they’re not. But they also need care and answers. We know that our medical system is not great at detecting early signs of illness, so there very well may be something physiologically wrong.”
She hopes her new book will do for chronic illness what Andrew Solomon’s The Noonday Demon: An Atlas of Depression (Scribner, 2001) did for that ailment. “He told a story that created a bridge between those suffering from depression and those who aren’t,” O’Rourke says. “William Styron did that too in Darkness Visible, and that’s partly what I’m trying to do. I’m not a doctor, and I’m not a historian. Mine is a very personal book that will provide some history of medicine and some cultural criticism about the ways our contemporary medical system affects the treatment of poorly understood diseases.”
The Disease of Our Age: Autoimmunity
“Nothing is more punitive than to give a disease a meaning—that meaning being invariably a moralistic one.”
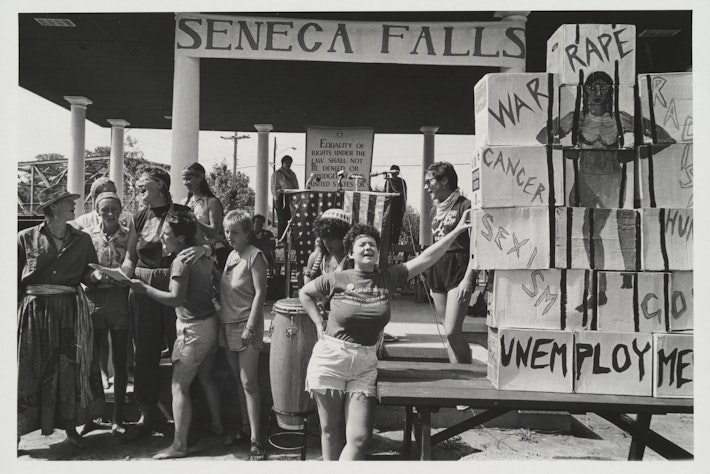
At her December fellow’s presentation, Megan O’Rourke invoked this statement from Susan Sontag’s book Illness as Metaphor (Farrar, Straus and Giroux, 1978). O’Rourke’s twist on the title is “illness as semaphore,” or sign. She believes that every age has its “representative, poorly understood, and highly symbolic disease” and that ours is autoimmunity—which occurs when the body attacks itself. We “read into” these diseases in a search for psychological origins that may or may not exist.
The largest category of chronic illness in the United States, autoimmunity includes celiac disease, Crohn’s disease, and rheumatoid arthritis and affects an estimated one in six people. These diseases are rising at what some researchers call epidemic rates, a rise that is not due just to increased diagnosis, O’Rourke said, citing a Johns Hopkins researcher.
It’s not clear what causes autoimmune disease, although researchers believe that part of the cause is genetic and part is environmental. These illnesses don’t occur as often in less-developed countries, which may indicate that autoimmunity is triggered by the proliferation of manmade chemicals since World War II and our increasingly hygienic environment. “It may be the case,” O’Rourke said, “that we have caused our own autoimmunity.”
Autoimmunity is as much a medical frontier, in her view, as syphilis or tuberculosis was in the 19th century. People with those diseases were denigrated and misunderstood long before their ailments were understood.